Impact Stories
Home > Impact Stories > Uncovering the extent of endometriosis
August 2024
Research is providing new insights into this crippling and hard-to-diagnose condition.
Recent boosts to research funding are highlighting knowledge gaps and the buffers that affected individuals often face in accessing treatment. In fact, Australia is the first country to have a comprehensive National Action Plan for Endometriosis.
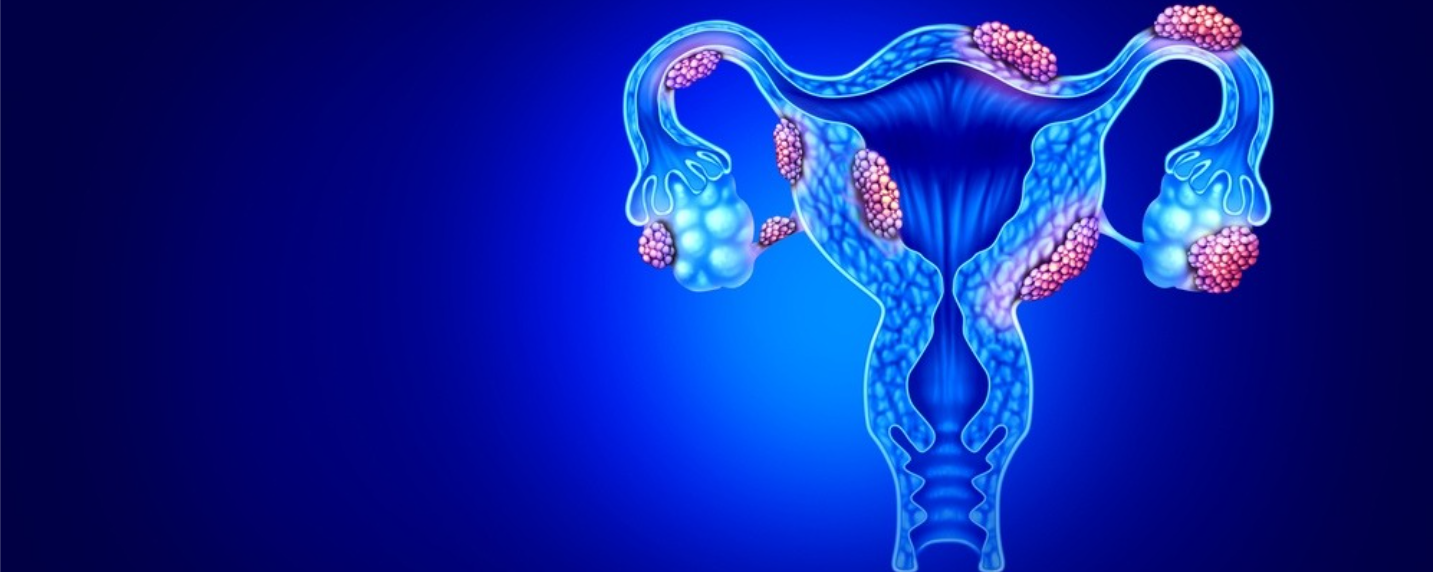
Endometriosis is an inflammatory disease where endometrial tissue is found outside of the uterus, on the ovaries, fallopian tubes or peritoneum, or less commonly in a woman’s lungs, stomach or colon. The symptoms are highly varied but include recurring severe pelvic pain, heavy bleeding and infertility. The location of endometrial tissue can affect the level of pain a woman feels.
Prevalence of endometriosis
Professor of Life Course Epidemiology, at The University of Queensland, Gita Mishra explained diagnostic delays are one of many challenges in estimating the disease prevalence.
“Despite increased awareness in the last five years, for many women, it may take 7-12 years for a diagnosis,” Professor Mishra says.
“Endometrial symptoms such as bloating and constipation also mimic many other disorders, such as Irritable bowel syndrome, while some women are asymptomatic.” Laparoscopy is the gold standard for diagnosis though practitioners are currently exploring less invasive methods for diagnosis, she confirms.
As Director of the Australian Longitudinal Study on Women’s Health (ALSWH), Professor Mishra says the study regularly collects data on around 57,000 Australian women. Funded by the Australian Government Department of Health and Aged Care, the study began in 1996 and is jointly managed by the University of Queensland and the University of Newcastle.
The ALSWH team link survey data with health data to glean the prevalence of women with endometriosis and other vital information. PHRN data linkage units, and other data custodians, across Australia assist with this linkage. Sharing recent findings, Professor Mishra explains one in seven women in the older cohort (born 1973 to 1978) were diagnosed with endometriosis by the age of 48. In the younger cohort (born 1989 to 1995), one in 11 women had endometriosis by their late 20s.
More research is needed to determine whether this difference in prevalence reflects the greater awareness of the disease or possibly a higher incidence.

Factors and co-morbidities future health research
Fifty to sixty per cent of endometriosis can be explained by genetic variance according to Professor Mishra. However, new research flags early life factors, such as low birth weight, may also be associated with the condition.
Other studies suggest endometriosis could be related to endocrine-disrupting chemicals, so her team is exploring air and water pollution, as well as occupational hazards as possible factors.
Common co-morbidities amongst endometriosis sufferers include back and joint pain, headaches, menstrual problems, anxiety, depression, constipation, inadequate sleep and low iron. These women are also more likely to experience miscarriages and gestational hypertension, to develop gestational diabetes mellitus, uterine fibroids or polyps. They are also more likely to develop polycystic ovary syndrome and have a baby born preterm of low birth weight.
The ALSWH survey data reveals sufferers report more frequent visits to the GP or specialist visits, before and after receiving a diagnosis compared to the controls.
These women are less likely to have a natural menopause and eight times more likely to have a surgical menopause (both ovaries removed) and at a younger age—all of which are associated with chronic conditions later in life.
The research team hope to produce an endometriosis risk calculator with clinical guidelines for health professionals. Recent interest in this condition, and subsequent funding boosts, should hasten diagnosis and quality care for affected women.
More information
PHRN Linkage Learning Webinar: Professor Gita Mishra on endometriosis
Privacy and security
Privacy protection and data security lie at the heart of the Population Health Research Network. The collection, use and disclosure of personal information by government agencies and other agencies are bound by strict legislative and regulatory conditions. Researchers wishing to access linked data must also adhere to stringent conditions, including ethics approval, data custodian approval and the development of a detailed data security plan.
Researchers are typically given access to a linked data set put together to meet the specific needs of their project. This de-identified data includes only the minimum information required for the research, such as age rather than date of birth. Government agencies handle personal information in highly secure environments. Data is delivered to researchers through a secure remote access facility, ensuring no information is stored on the researcher’s personal computer or their institutional network.
Researchers cannot export raw data from this system, only their analyses, and these are checked. Researchers must only use the data for the approved purpose and are not allowed to link any other information. At the conclusion of the project, all data must be destroyed or returned. Penalties for researchers and government employees can include criminal conviction, jail time or substantial fines. In the more than ten years since the network began, there has never been a breach.

